The doctor - patient relationship framed around smoking cessation
Bonus: three phrases a patient can use to empower the relationship with their doctor
Human use of tobacco. Risks/harms of smoking. 1964 American Surgeon General warning. Smoking cessation through scare. Smoking cessation through education. Smoking cessation through motivational interviewing. Medicines for cessation. Framing the doctor-patient relationship. Three empowering patient phrases. Mention of determinism.
Tobacco’s success
Humanity has used tobacco for more than 12,000 years. Whether chewed or smoked, tobacco is associated with a good feeling. The crop was used in some American colonies as currency. The financial success of tobacco is a big part of the historical Transatlantic slave trade. As global technologies improved, so did techniques for preparing tobacco for human use. Tobacco cigarettes could be factory produced by the late 19th century. It became socially acceptable for women to smoke in the early 20th century. Smoking had become a norm and nearly half of American adults were cigarette smokers by the 1950s.
Risks and harms of smoking — why doctor’s oppose smoking
Nicotine is the pleasurable psychoactive component of tobacco. It has stimulating effects and also increases activation of reward pathways. The reward activation leads to reinforcement of use of nicotine. As a user maintains chronic exposure to nicotine, the reward becomes less prominent and the brain may become more sensitive to stress and stress reactions. This manifests as anxiety and drug-seeking behavior. Nicotine discontinuation leads to a bad feeling, which inevitably reinforces use of nicotine.
Unfortunately, the nicotine delivery system in cigarettes is associated with significant harm. About half of all chronic tobacco smokers will die of a smoking related illness. Breathing in the products of combustion is breathing in poison. The nicotine in a cigarette is delivered into the body via tar that sits in the lung. The tar is foreign so the body reacts to get rid of the tar, but not fast enough — the tar sits in the lung causing chronic cough. Because smoke floats in the air, cigarette smoking exposes others to breathing poison (and we tend to spend the most time around people we love).
Smoking increases risk of heart disease, lung disease, stroke, diabetes, and vascular disease. Notably, these chronic conditions all are associated with a significant decrease in quality and quantity of life.
Then there is cancer. Ask any child and they will associate smoking with cancer. Most notably smoking is associated with lung cancer, but also throat/mouth, esophagus, stomach, bladder, kidney, pancreas, AML and more. Cancer gets a lot of attention, and it should, but I argue that smoking is hazardous enough to recommend against even if cancer risk is set aside.
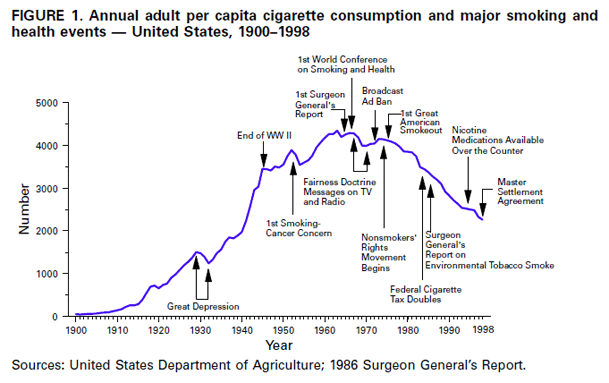
Surgeon General’s report — the beginning of the decline
The health risks of smoking had been revealed prior to the 1960s, but in 1964 the US Surgeon General announced the link between smoking and lung cancer. This was a time in America that cancer was getting more attention in the mind of the public. Many infectious diseases had become preventable or curable. Heart disease had become the number one killer of Americans in 1950, and cancer the second leading cause of death since 1933. The year after the Surgeon General’s warning marked the top of the curve of adult smokers in the USA. The seven decades since has seen an undeniable decline in smoking. Concerted public health information campaigns, taxation, disallowing advertisement, challenging big tobacco, smoking cessation aids, and psychotherapeutic techniques all played a roll in bringing smoking prevalence down to a stunning 11% of US adults in 2024. The social image of smoking has changed from glamorous to unhealthy.
Models for smoking cessation — how the doctor interacts with the patient
Human behavior is complex. The human mind is not a rational machine. Rather, behaviors interplay with emotion, beliefs, and subconscious habits. Preventing exposure to nicotinic products is much more effective at reducing smoking rates than encouraging existing smokers to quit. Prevention is king, but helping existing people is just as important. Doctors began to command “quit” because smoking is so harmful to health. Some people probably did quit because doc said so, but quitting is difficult.
A new conundrum had emerged: Let’s imagine a doctor-patient relationship wherein both parties accept smoking is harmful. Doctor says “quit,” patient says “yes sir.” A few months go by, patient returns to doctor and patient smells like tobacco smoke. Doctor says “quit,” patient says “can do.” A year goes by and nothing has changed. A powerlessness has been revealed.
Cynical humor is a common reaction to frustration, but I retort that impossible problems are the most worthwhile. The doctor wants the patient to have improvement and the patient wants to have improvement, but the power of nicotine is great.
What would you do if you were the doctor?
Scare tactic
Some clinicians resorted to scare tactics. If the possible outcomes of cancer, stroke, etc. are scary enough, and the patient wants to avoid those outcomes, then the negative emotion of fear might overpower the bad feeling of nicotine’s absence. Generally this approach feels bad and leads to even more smoking to make the bad feeling go away. We call that a backfire.
Education
Some clinicians engaged patients in education about risks and harms. They discussed the downsides of smoking. The thought is intuitive: if a person knows how smoking is so very harmful in every way, they will naturally give it up! However, focusing on education with the patient leads to feelings of guilt for engaging in self-destructive behavior. An educated, guilty smoker. Education is useful for prevention of new smokers. Clinician education is vital for empowering clinicians to understand the stakes so that they may be persistent with the most effective anti-smoking interventions.
Motivational interviewing
Quitting is difficult. Most people are future quitters with a bit of prompting and priming. First, people find enjoyment in smoking, so it is no fair to describe smoking as all bad. Smoking enhances relaxation, allows for a mental break to enjoy the outdoors, and is an activity that increases social interactions. Motivational interviewing is about understanding the position of the smoker and encouraging change through rapport and compassion when the time is right. This means treating cigarettes with fairness, acknowledging that quitting is difficult (whoever quits gets a lot of credit), encouraging a change when ready, making the process as least difficult as possible, and always trying again instead of getting frustrated.
Motivational interviewing and motivational enhancement therapy is process focused. A clinician can work a process with a patient indefinitely, there is never a need to get frustrated or stop the process. Motivational interviewing to assess readiness for change and motivational enhancement remain the most effective clinical approaches for smoking cessation.
Medicine
Medicine aids for smoking cessation can help quite a bit. The perfect medicine has not yet been discovered, but the current smoking cessation aids are pretty good. There are a bevy of nicotine replacements including transdermal patches, lozenges, and inhaled powders. Later, nicotine vaporizers came to market as smokeless nicotine products, but unfortunately were marketed to non-smokers.
Access to nicotine replacements proved that a habit with smoking is much more than nicotine addiction. Cravings seem to come and go for the rest of a person’s life, and being around tobacco will be a risk factor toward relapse even years after quitting. A quitter’s routines, relationships, and places they used to smoke could lead them back to smoking, even months after nicotine replacement had been successful.
Some people noticed it was easier to quit when taking an antidepressant, bupropion. Eventually it was FDA approved for smoking cessation. One could continue taking bupropion long after quitting
Currently, the most effect medicine for quitting is varenicline. It can be started before the target quit date and continued for several months after quitting. The downside is cost and some side effects, but this drug is pretty amazing. Smoking is very addictive and quitting is very difficult, even with the best medicine.
A doctor in training circa early 2000s — introduction to motivational interviewing
The traditional medical school model is year one basic science, year two pathology, year three clinical rotations, year four more clinical rotations along with electives and residency applications. Training in motivational interviewing for smoking cessation occurred in the first week of medical school. The message is “anti-smoking is too important to let it wait until week two of medical school.” The upshot of this early training was exposure to a thought process about ideal framing of the doctor-patient relationship. This model creates a therapeutic alliance, builds rapport, and then uses the warmth of the relationship to guide a patient into considering the most effective treatments. The motivational interview identifies resistances then overcomes barriers and obstacles with persistence and compassion.
Everyone wants to feel good and not bad. Most people will agree they also want to feel good and not bad in the future. Change is hard. The patient will trust the doctor when the patient feels heard. Trust is the investment of change. The doctor’s duty is to identify the most effective changes and make the changes as accessible as possible. The patient’s duty is to be present and report back as honestly as possible.
Beyond smoking cessation — three phrases to enhance personal healthcare
Smoking is a socioeconomic phenomenon. Nobody would ever have smoked without access to tobacco (a tautology worth repeating). The medical model is a systematic process of ruling out wrong diagnoses, identifying true diagnoses, intervening with medical science, managing expectations, and encouraging the patient to maintain engagement in the process. There are a lot of versions of good outcomes. Patients can enhance the doctor-patient relationship too by tapping into what made the doc become a doc.
The following patient statements, if sincere, will foster a warmer doctor-patient relationship.
Phrase #1 “I am scared and I do not know what to do.”
It feels so much better to give help than to receive it. The clinician enjoys the feeling of helping others. However, being the patient is often scary, overwhelming, unreal, expensive, confusing, irritating, and rushed. Asking for help, directly if possible, facilitates a slower dynamic. Hearing someone is scared gives the healer a pause. Hearing someone does not know what to do helps the healer slow down and ensure the patient gets the right information. We communicate an expectation with every word/behavior. It is good to expect help from the doctor. Part of the encounter should be learning what to expect and what to do next.
Phrase #2 “I like working with you doctor, you really get me.”
Liking someone makes us more likeable. Likeable people get more time and attention. Doctors are biologic organisms and not robots. Professionals have biases, even if they are trained to reduce biases. A little flattery goes a long way. It is unsanctimonious to admit it, but it works.
Phrase #3 “Thank you for helping me, but this is really hard. Is there another way?”
We can be grateful and open to change at the same time. Doctoring is the business of what works. It is normal to wish a problem did not exist, but the doctor will encourage action. Asking about options can be part of accepting a change and this question might also lead to a more open discussion.
Closing remarks
A doctor helping a patient become motivated to quit smoking is the heart of doctoring. The doctor’s incentive is the patient’s health, the patient’s incentive is their own health, the pathway forward is a change in patient behavior, and the results are invisible. It requires trust that quitting is worthwhile. A doctor who views smoking and quitting as deterministic will be more effective than a doctor who views smoking and quitting as a characteristic. More to come on determinism in healthcare.